Can Rolfing help Plantar Fasciitis?
What is Plantar Fasciitis?
Plantar Fasciitis is a pain condition characterised by pain in the sole of the foot near the heel which is often worse after rest but gets gradually better with movement.
There is some dispute over the whether Plantar Fasciitis is in fact an inflammatory condition as some believe the pain is predominantly the result of micro tears in the plantar fascia, rather than inflammation, in which case Plantar Faciosis would be the appropriate term. My own view is that it is plausible that both inflammation and micro tears can coexist in the condition. Nevertheless, I will refer to the condition as Plantar Fasciitis.
The Rolfing Approach
Rolfing can be extremely effective in reducing or eliminating pain from Plantar Fasciitis, especially when the pain is a result of excessive muscle contraction.
In any attempt to resolve musculoskeletal pain conditions such as Plantar Fasciitis, it is important to achieve structural integrity and balance in your myofascial system — Rolfing Structural Integration aims to do this.
The myofascial system consists of muscle (myo-) and fascia, which is collagenous connective tissue that permeates your body, wrapping individual muscles, bundles of muscles and organs.
Your myofascial system is a holistic reciprocal tension network rather like a tensegrity structure. In this network muscles work synergistically to enable you to move and maintain your posture against the force of gravity. Because of the reciprocal tension dynamics in this system, stress in one area of your body, such as the plantar fascia, is distributed throughout your whole body.
Therefore the best approach to resolve Plantar Fasciitis is to address not only the local area at the site of your pain, but also to supplement this by correcting any imbalances in the surrounding myofascial units, in particular your lower legs.
Identifying the cause of your Plantar Fasciitis
Part of the treatment involves identifying the probable cause of the pain. Is there some bodily action in the your lifestyle repeated on a regular basis which can logically be the source of the condition? Common causes can be:
Tight-fitting shoes
Repetitive sports activities
Regular driving
Prolonged standing, especially on tip-toes
Once the cause is identified preventative measures can be taken to eliminate or reduce the offending action.
Treatment of relevant myofascia
Where the Plantar Fasciitis is caused by excessive concentric contraction of the muscles and tension in the surrounding fascia and fascial bags, the goal is to release such tension by working on the relevant areas.
1. Gastrocnemius and Soleus

Tension in the calf muscles can feed into the plantar fascia, especially around the heel and Achilles tendon so work on the muscles and around the tendon itself can be effective in reducing the pain.
2. Fibularii/Peroneals

Additionally the muscles on the side of the calf, called the Fibularii, or Peroneals (Longus and Brevis) might be contributing to the Plantar Fasciitis — these muscles are used for standing on tiptoes or pressing the pedals in driving (plantar flexion) and also for foot eversion/pronation, which is where you move the outside of your foot up and away from the ground. They can be released directly in the Rolfing treatment along with the associated retinacula.
3. Tibialis Anterior and Posterior
A contributing cause of Plantar Fasciitis can be imbalances in the arches of your feet — arches which are either too high or too low. While excessive tension in the Fibularii can cause flat feet, high arches can be caused by the Tibialis Anterior and Posterior muscles, so it is worth checking for this and treating these muscles appropriately with a view to restoring balance.
4. Hamstrings

There is a direct continuation from the Fibularis Longus into the Biceps Femoris, so it is also important to check this lateral hamstring for excessive tension and treat it accordingly. Equally the calf muscles connect to all three hamstrings in a myofascial chain that goes up the back of your body, so it is appropriate to treat any imbalances found in the hamstrings on both the inside and outside of your leg.
5. Plantar Fascia

Obviously a key part of the treatment for Plantar Fasciitis is releasing tension in the plantar fascia itself. In my experience this can be extremely effective although sensitivity and appropriate calibration of touch is crucial. First, it is important to work towards the heel, not away from it, in order to avoid worsening the micro tears close to the heel or exacerbating any inflammation.
Second, when working directly on the site of the pain, which is usually close to the heel, a work-and-test approach is the best option. Namely, after applying some pressure onto the painful site you will be asked to give feedback straight after the procedure, both on the table and in walking, in order to test the effectiveness or any adverse reaction. In the case of repeated treatments in two or more sessions, monitoring the progress of the condition after each session and reporting any increase or decrease in pain provides vital information in helping to decide how to proceed with treatment.
Calf Stretches
In the case of tight calf muscles it is advisable to support the treatment by doing calf stretches to counteract the muscle contraction. My preferred calf stretch is the ‘telephone directory’ stretch. This is anachronistically named as few people have telephone directories any more, but a nice thick book approximating to the old Yellow Pages (UK) will suffice.
The book (soft covers are better than hard covers) is placed in front of a wall so the furthest edge is about 50cm from the wall. You step on this edge and lean forward, putting your hands on the wall and letting your heel hang back off the book’s edge. This will give a stretch to your calf muscles which you can control by how much you allow your heel to hang off the edge of the book. This stretch is similar to its variant where you hang your heels off the edge of a stair or step, but the telephone directory stretch has the additional advantage of enabling you to carefully control and modulate the stretch.
Another advantage of the telephone directory stretch is that it allows you to isolate either of the two calf muscles:
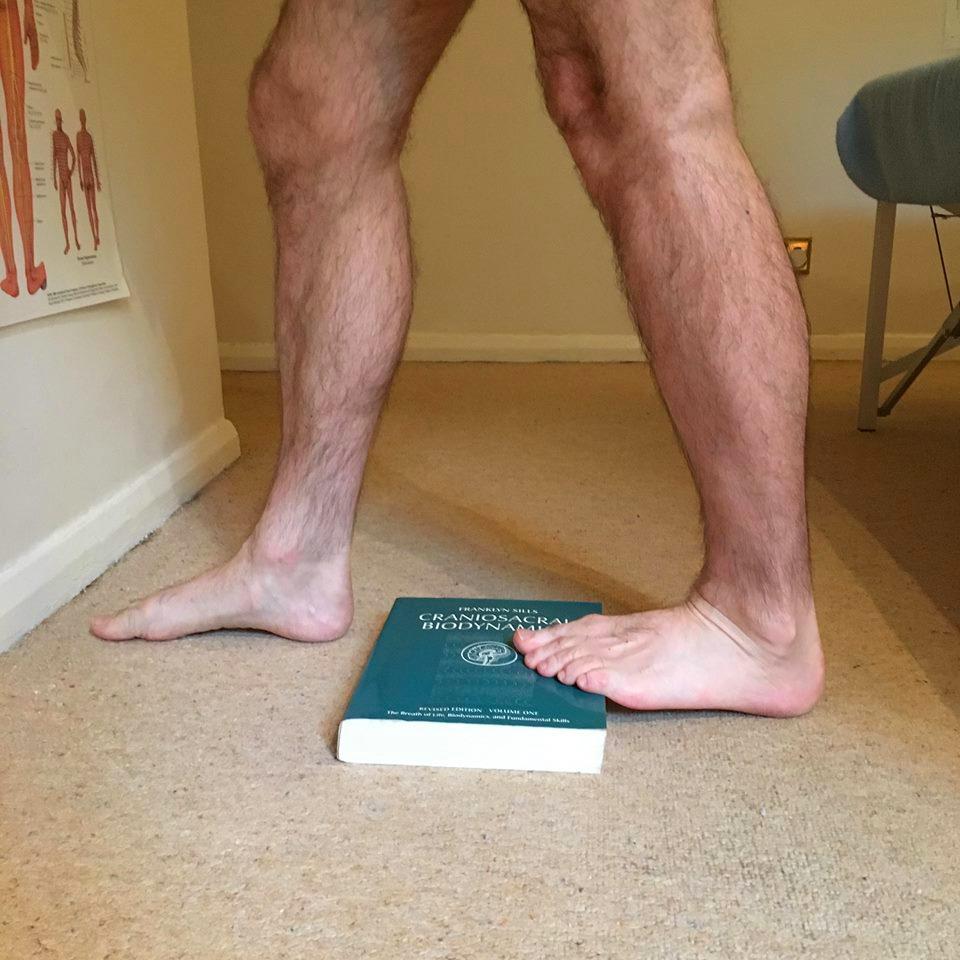
The Gastrocnemius is stretched by keeping your knee straight
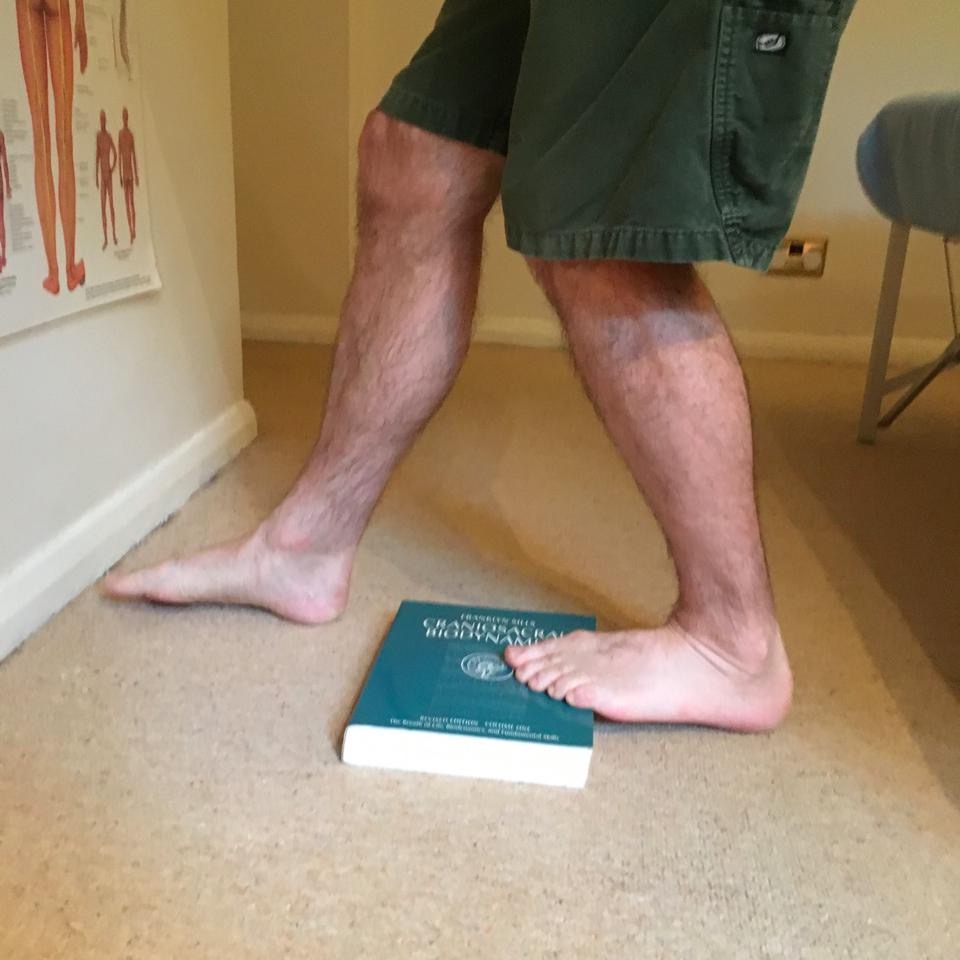
The Soleus is stretched if you bend your knee
Slow stretching works best: get to the point where you can feel the stretch happening and it is not too painful, hold the stretch, breathe deeply and slowly and wait for the point where you can increase the stretch a little without increasing the pain — the pain should lessen, not increase.
The aim is to find the ‘sweet spot’ in the stretch, where you are challenging the tissue but not going past the point where your stretch reflex kicks in and suddenly tightens the muscle.
Breathe, hold the stretch, wait for the softening, then take the stretch to the next barrier.
As with all stretches be aware of your body’s sensations and don’t push it too far. Test the results by walking afterwards: the desired result is a reduction in the heel pain, not an increase.
Conclusion
The Rolfing approach combines direct work on the site of the pain along with a careful examination and treatment of the most relevant muscle groups and myofascial units which are connected to the painful area. In any pain condition addressing the global myofascial network along with the local area of the pain gives the best chance of pain resolution. Plantar Fasciitis is no different.
Careful, calibrated work on the plantar fascia close to the area of pain, informed by ongoing feedback, is supported by treatment of other relevant areas such as the calf muscles, Fibularii, Tibialis muscles, and hamstrings. This is supplemented by manageable lifestyle changes to prevent future occurrence of the condition and targeted stretching after the Rolfing treatment.
Click here to read more https://www.rolfing-london.co.uk/about-me/

